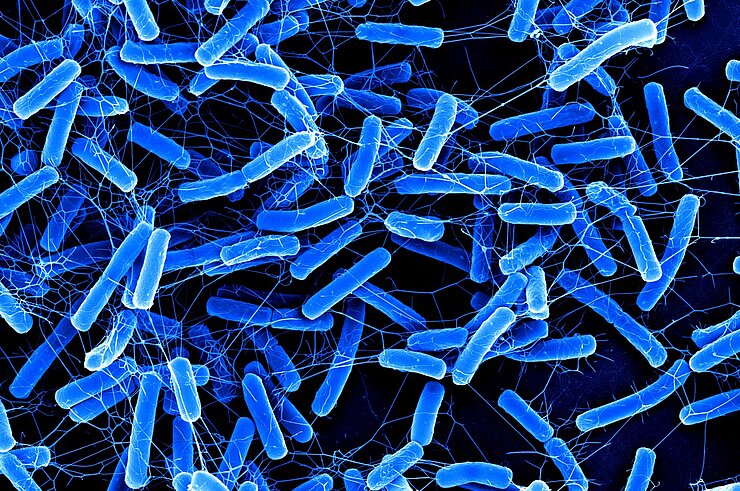
Clostridioides difficile
In recent years, Clostridioides difficile ( formerly Clostridium difficile), a gram-positive bacterium, has become one of the most common causes of diarrhoeal diseases that are triggered by antibiotics. This germ is present in the intestines of healthy people and animals quite naturally. It causes damage only if the normal intestinal flora - i.e. the composition of bacteria in the intestines - is disrupted.
This happens mainly upon treatment with antibiotics. During the treatment, bacteria competing with Clostridioides difficile are killed specifically. Once its competitors are gone, the pathogen can proliferate more strongly than usual and the risk of infection increases. Accordingly, the germ is a hazard mainly in places, in which many antibiotics are applied, for example in hospitals.
Route of infection
The infection by Clostridioides difficile usually proceeds through a smear infection from human to human caused by the uptake of environment-resistant spores. The microbes are passed on through minute trace amounts of faeces on the hands of ill people. Eventually, the pathogen manages to transfer from the hand to the mouth. But the germs can also survive outside of the gastrointestinal tract, namely in the form of spores, which means that they can be transmitted via objects as well. Touching a door handle that has a pathogen sticking to it may be sufficient for transmission.
The ability to form spores is associated with yet another advantage, because the spores allow the bacterium to hide itself from antibiotics and other external influences. That makes these bacteria particularly resistant and persistent.
A new hazard
And yet, the bacterium was considered to be no more than a minor hazard until recently. Only in the past 10 to 15 years, the rate of infections caused by this germ has been on the rise. The reasons for this are twofold.
Firstly, due to mutations in the genome of the bacterium, more toxins are produced than used to be the case. The toxins paralyse the intestinal wall and, in a worst-case scenario, lead to a balloon-like distention of the large intestine, which is called "toxic megacolon". This results in severe, in some cases even fatal, damage to the intestine.
Another reason for Clostridioides difficile to emerge as a new hazard is the ability of the bacterium to develop resistance to certain antibiotics. Within but a short time, two different strains of the pathogen have become resistant to fluoroquinolones. This class of antibiotics was used commonly in the 1990s and 2000s, mainly in the USA. And this is where the resistant strains originated, as has recently been shown by researchers.
A global issue
The researchers analysed the genes of the resistant strains and were thus able to trace both the origin and the distribution of the germs. The pathogen succeeded to spread throughout the world within just a few years. This rapid spread is due to the modern lifestyle of humans. Basically, the resistant Clostridioides strains can rely on the public transportation system for spreading. The resistance of the bacteria is another advantage promoting their rapid spreading.
Infection control based on hygiene measures
Clostridioides difficile is becoming a true problem, especially in hospitals. In order to solve this problem in the long-term, a variety of measures is required. Firstly, the use of antibiotics must be subjected to stronger controls and these medications must be used only if there is absolutely no other choice. Secondly, improved hygiene measures can minimise the transmission rates and thus prevent the bacteria from spreading.
Researchers also see much potential in the development of vaccines for containment of the problem. Similar to many other nosocomial germs, preventive and hygiene measures could make a major contribution to successfully controlling the much-feared germs. True to the motto: Forewarned is forearmed.
Involved research groups
-
Microbial Immune Regulation
 Prof Dr Till Strowig
Prof Dr Till Strowig -
RNA Biology of gram-positive bacteria
 Prof Dr Franziska Faber
Prof Dr Franziska Faber