Emerging Diseases – A challenge for research, medicine and society
To eradicate infectious diseases forever: This vision is likely to remain wishful thinking. Even if medicine were able to find a cure for each individual pathogen, the victory would most likely be short-lived. Sooner or later, a new virus or a new bacterium would arise for which no cure is available.
New pathogens - and therefore new diseases - keep arising. The ever-active forces of evolution make sure that Viruses and bacteria keep producing new genetic variants. Sometimes they cross biological borders between species and suddenly infect people instead of their former common hosts or they transition from harmless dwellers in our environment to become dangerous killers. Since the human immune system is not prepared for these new germs and has no defence against them, some of them spread very rapidly and cause previously unknown epidemics.
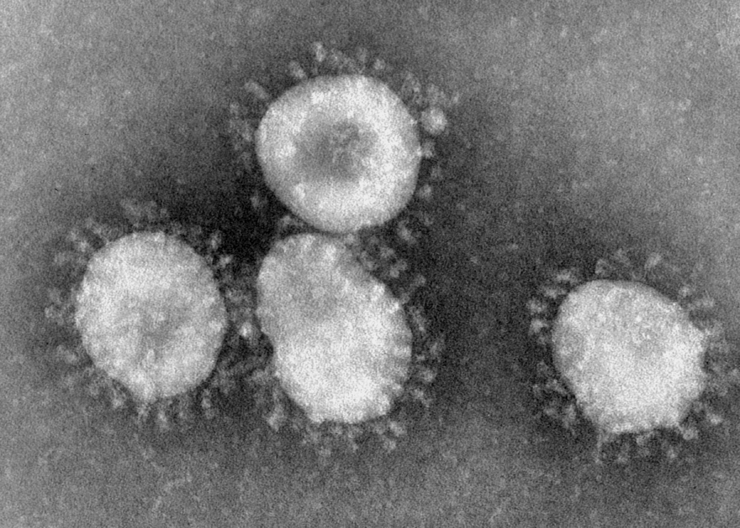
For example, one such new disease became a major global threat in the spring of 2003 - and there wasn't even a name for it in the beginning. Cases of "atypical pneumonia", which is the term initially used by physicians to refer to the phenomenon, occurred at increasing rates in eastern Asia and began to spread to other continents as well. The World Health Organization classified the highly contagious and often fatal lung infection as a novel Epidemic and named it: "Severe Acute Respiratory Syndrome", or, for short: SARS.
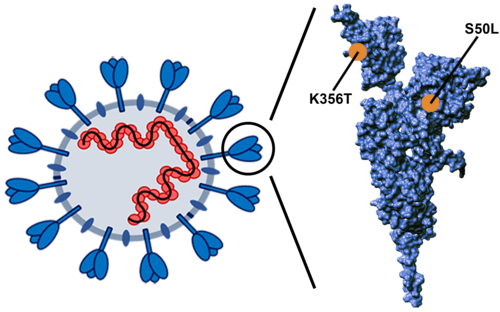
It became evident later on that the virus causing SARS-Epidemic was indeed novel - at least in humans. It belonged to the Corona viruses, a group that also includes pathogens causing common head colds. But, in contrast to these, it used to infect animals only - until now. The SARS virus probably originated from bats and, due to a genetic change, acquired the ability to infect humans as well.
Some 8,000 people became afflicted SARS and 700 died before the Epidemic was contained in the summer of 2003 by quarantine measures and specific monitoring of airports.
Special features of emerging diseases
In many ways, SARS is considered to be typical of an " Emerging Disease", i.e. a newly arising disease. Similar to the SARS Corona virus, many newly emerging pathogens originate from animals. These so-called Zoonoses, which can become manifest in humans as well as in animals, include much-feared diseases such as AIDS and Ebola, but also the annually recurring Influenza or influenza.
Influenza Viruses have a vast reservoir of many subtypes in aquatic birds. This is a major problem because it means that we can never eradicate the virus completely.
In addition, the influenza virus keeps producing new genetic variants at very short intervals. If one of these variants crosses the barrier between species and infects human lung tissue and then - in a second step - also manages to spread from one human to another, then this often leads to a Pandemic, i.e. an infection that spreads on a global level. "And this has happened a number of times in history," says Schughart.
But animals are not the only possible origin of a novel infectious disease: Sometimes, a germ that is common in humans and elicits no more than mild symptoms, suddenly becomes aggressive and even life-threatening as a result of genetic changes. For example, the EHEC outbreak in Northern Germany in 2011 was caused by a highly pathogenic strain of the otherwise harmless intestinal bacterium, Escherichia coli (E.coli O157:H7). Presumably, the exchange of genetic material between different bacteria in the human intestines had given rise to the aggressive germ.
As disturbing as the continuous threat by "Emerging Diseases" may be - medicine and society are by no means defence-less. One important aspect is the continuous monitoring of the "high-risk candidates" amongst Viruses and bacteria, i.e. those germs, which are most likely to undergo hazardous changes. This approach is successful, at least in part, in influenza Influenza: Often it is possible to calculate ahead of time, which genetic variants will spread in the near future, and this knowledge can be used in the development of the vaccine for the next flu season.
Other antidotes can be delivered - in the long-term - by targeted basic research: Knowing what happens in detail when Viruses or bacteria infect the human body also uncovers the first reference points for how to specifically block that process.
"The better we understand the underlying mechanisms of infections, the quicker we can respond when we face the next new infectious disease.", says HZI scientist Klaus Schughart. And this can happen any time, Schughart says: "The question is not whether or not the next Pandemic will happen - but rather, when will it happen.“
(mbn)
Involved research groups
-
Pathogen Evolution
 Prof Dr Sébastien Calvignac-Spencer
Prof Dr Sébastien Calvignac-Spencer -
Evolutionary Community Ecology
 Dr Jan Frederik Gogarten
Dr Jan Frederik Gogarten -
Biosafety Level 3 Laboratory
 Dr Kai Schulze
Dr Kai Schulze -
Laboratory for Virus-Host Co-Evolution
 Dr Max Kellner
Dr Max Kellner -
Ecology and Emergence of Zoonotic Diseases
 Prof Dr Fabian Leendertz
Prof Dr Fabian Leendertz -
Laboratory of Transmission Immunology
 Dr Julia Port
Dr Julia Port