Individualized Infection Medicine
For some years now, the buzzword "individualized medicine" (often also referred to as "personalized medicine" or "precision medicine") has been the subject of heated debate in research, clinical practice, industry and healthcare policy. What is meant by this term?
Around ten years ago, advanced cases of malignant melanoma were usually treated with chemotherapy. However, this standard procedure does not work equally effectively for all patients. Today, therapy for advanced melanomas is often preceded by a genetic analysis of the tumor cells. Certain mutations can lead to increased cell growth and thus drive the growth of the tumor. The doctors administer an active substance to the patients concerned that blocks the signal for cell division. This treatment can significantly prolong the survival time of patients, but also causes troublesome side effects such as joint pain and skin changes. For this reason, the drug is not used in patients without the mutation in question.
In some other cancers, such as stomach and breast tumors, some patients show potential drug targets on the surfaces of their cells, while others do not. A different treatment makes sense for each patient group.
Such differentiation according to the specific requirements of the individual patient is a central element of individualized medicine. In simple terms, treatment is preceded by diagnostic tests, the results of which are intended to enable a therapy or prevention that is precisely tailored to the patient and their clinical picture.
"The basic idea is of course not entirely new," explains Prof Michael Manns, internist and gastroenterologist at Hannover Medical School (MHH) and Clinical Director of the HZI.
Medicine has always strived to identify the specific characteristics of each individual patient in order to provide them with the best possible treatment. However, the technical possibilities for this have improved enormously in recent years. Their use now makes it possible to take diagnostics to a whole new level.
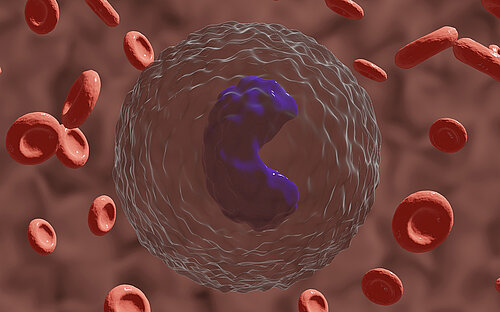
It often only takes a simple blood sample to create a detailed snapshot using modern technologies that can provide information about molecular processes in humans or pathogens. In addition to the analysis of all the genes in an organism - genomics for short - the analysis of other biomolecules has also made enormous progress and can be applied using automated processes in high-throughput procedures. Transcriptomics provides doctors and bioscientists with data on which genes are actually being transcribed - and how intensively. Proteomics reveals which different protein molecules occur as building blocks and biological catalysts in cells and tissues. Metabolomics records the totality of all metabolic products in the organism.
The above-mentioned techniques, often summarized under the collective term "omics" due to their common ending, now make a huge flood of data available - in conjunction with increasingly powerful computer systems. The challenge now is to process this data and link it together in such a way that predictions can be derived from it. If this succeeds, the individual risks and susceptibilities of each person can be determined far more quickly and accurately than would have been thought possible just a few years ago. The resulting targeted preventive or therapeutic measures can lead to better treatment success, avoid unnecessary side effects and reduce costs.
"By elucidating the function of a molecule, for example, we can learn a lot about the development of a disease and thus improve prevention or treatment," says PD Frank Pessler, physician and scientist at TWINCORE in Hanover. "The remarkable thing, however, is that you don't necessarily have to fully understand its function in order to use it to diagnose a disease." Ideally, the connection is simple: if a certain molecule can be detected in the body, disease X is present or therapy Y is recommended. Such molecules - or other meaningful findings that can be detected by means of a diagnosis - are referred to as biomarkers.
With the help of biomarkers, but also other methods (e.g. physical procedures, classic anamnesis), patients can be divided into groups for which certain therapeutic or preventive approaches make sense. Experts call this classification stratification. An individually adapted treatment derived from this promises - in comparison to a uniform therapy for all patients ("one-fits-all") - to largely avoid serious side effects and increase effectiveness (see Fig. 1 ). Stratification has also been practiced in medicine for a long time:
However, individualized medicine claims to make this classification on the basis of verifiable, scientifically sound criteria - i.e. evidence-based rather than based on experience. This is intended to make it more precise and effective.
The individualized approach has now found its way into clinical practice, and the use of biomarkers for the targeted identification of suitable treatment is becoming increasingly widespread (see Fig. 2). Of all novel drugs approved in the US in 2015, more than 25 percent were personalized medicines: they are only used in conjunction with diagnostic tests for specific biomarkers.
Cancer medicine in particular has developed strongly in the direction of individualization, as the examples mentioned above show. "Today, cancer treatment is often preceded by a molecular genetic examination of the tumor in order to be able to combat it with tailored weapons," says Michael Manns.
There are also already individualized therapies for the treatment of infections. One of the most important drugs in HIV therapy, for example, leads to severe, sometimes life-threatening side effects in some patients. A certain genetic predisposition is responsible for this. The presence of this predisposition and therefore an increased risk of corresponding side effects is therefore checked before treatment. In this case, the treating physicians initiate an alternative therapy.
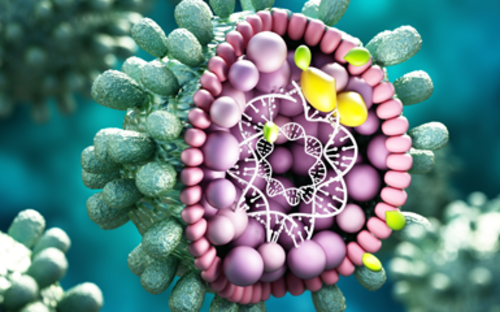
The treatment regimen for chronic hepatitis C is also individually adapted. It is not only patient parameters such as certain pre-treatments that are used to draw up the treatment plan, but also the pathogens, which are divided into groups and combated using different methods. Depending on the genetic type of hepatitis C virus present, a different approach is necessary.
However, the possibilities of individualization in the treatment of infections are far more diverse and have not yet been nearly exhausted. Together with the MHH, the HZI has therefore founded its own institute dedicated to investigating the individual profiles of people and pathogens: the Centre for Individualized Infection Medicine (CIIM) in Hanover, headed by Michael Manns as Director.
The CIIM aims to bring together clinical and research expertise in interdisciplinary projects in order to develop new concepts for customized treatments in infection medicine. The CIIM is currently a virtual network. The infrastructure is to be pooled in a planned new research building, thus creating the ideal conditions for an intensive exchange between the participating disciplines.
The doctors and scientists at CIIM are looking for biomarkers that provide information about individual risks and characteristics of patients and for methods to quickly find out more about the threat potential and weak points of individual strains of bacteria and viruses. In future, they want to use innovative tests to easily check the effectiveness of vaccinations and predict the tolerability of therapies.
The long-term vision is to be able to create an individual profile of each patient with an infectious disease. It should then be possible to derive the most suitable therapy from this profile. There is still a long way to go until then. But I am sure that we at CIIM can make a significant contribution.
References
Figure 2: Personalized Medicine Coalition. The Case for Personalized Medicine. 2011. | Personalized Medicine Coalition. The Case for Personalized Medicine. 2014. | Tufts Center for the Study of Drug Development. Personalized Medicine Is Playing a Growing Role in Development Pipelines. Impact Report, 12 (November/December 2010): 6. | PMC Progress Report 2015 and 2016: Personalized Medicine at FDA.
Further information
Involved research groups
-
Computational Biology for Individualised Medicine
 Prof Dr Yang Li
Prof Dr Yang Li -
Personalised Immunotherapy
 Prof Dr Kathrin de la Rosa
Prof Dr Kathrin de la Rosa