Staphylococcus aureus - Danger from the nose
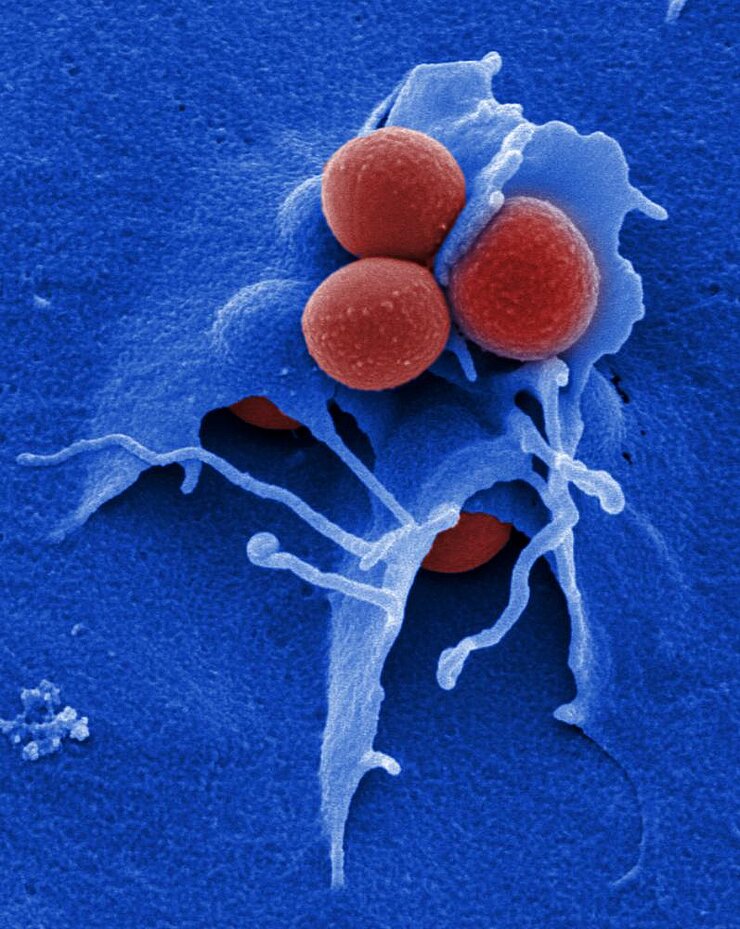
Staphylococci bacteria are ubiquitous. This also applies for the sadly famous Staphylococcus aureus. We take it for walks on the surface of our skin, it lives in our airways, and we pass it on to others when we shake hands or sneeze. Roughly one-third to one-quarter of all people are living with this germ – without so recognizing it and without creating any trouble.
Staphylococci bacteria are ubiquitous. This also applies for the sadly famous Staphylococcus aureus. We take it for walks on the surface of our skin, it lives in our airways, and we pass it on to others when we shake hands or sneeze. Roughly one-third to one-quarter of all people are living with this germ – without so much as being aware of it or experiencing any ill effects.
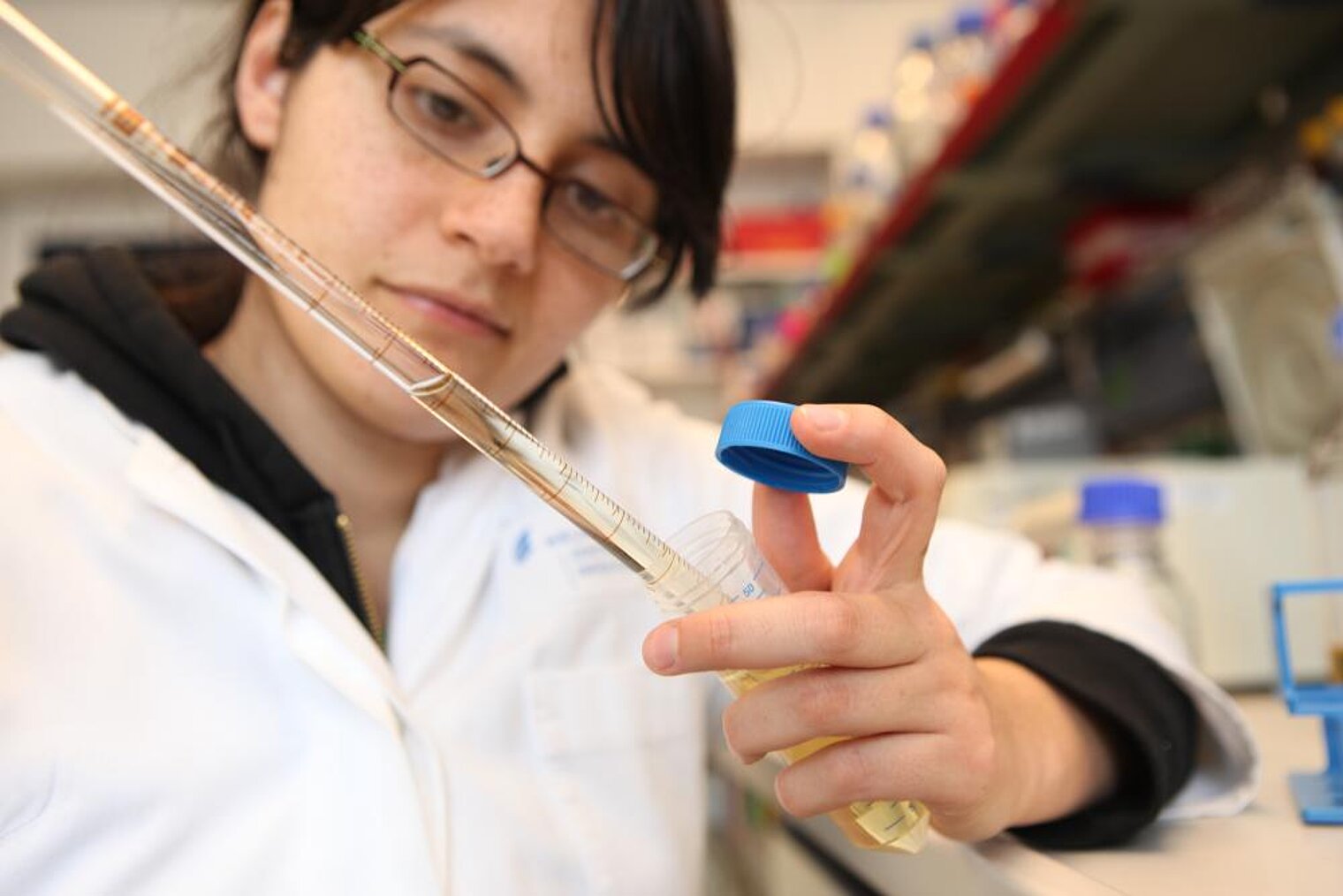
However, in the event that a carrier’s immune system becomes compromised, the unsuspecting companion quickly becomes virulent. The outcome: wound infections, muscle diseases, even deadly sepsis. In order to effectively ward off Staphylococcus aureus infections in the future, scientists at the Helmholtz Centre for Infection Research are studying different aspects of staphylococci infections.
Living in jolly good company
The germs form complex communities with other bacteria and are especially fond of colonising our nasal passages. This particular reservoir of staphylococci has long since been considered the primary source for serious wound infections. One grab of the nose gets Staphylococcus aureus in direct contact with the wound, paving the way for an infection.
In this context, the chronic wounds of diabetic patients represent an especially serious dilemma. Our scientists study the processes of infection of bacteria in their “nasal latency“ stage and in diabetic wounds. They also conduct epidemiological studies to track the spread of germs in the healthy population. Of particular interest is the identification of risk factors for Staphylococcus aureus colonisation of the nose – in order to come up with new therapeutic approaches for getting rid of the germ both inside the nose and in the wounds.
Infections – an interplay
The interplay between pathogen and immune system is critical for the metamorphosis from friendly companion to vicious attacker. If given the chance, the bacteria will trigger an infection and the beleaguered organism must get outside help – help that, for the time being, is still offered through antibiotic treatment, which is quickly losing its effectiveness. The bacteria are also adept at rapidly responding to newly developed drugs with ever newly evolved defense strategies.
Such helplessness vis-à-vis a virulent pathogen of the caliber of Staphylococcus aureus can quickly become life-threatening when the germs literally flood the organism and lead to sepsis. That is why our scientists are constantly on the look-out for permanent ways around such bacterial evasion tactics. One option: attenuate the pathogen instead of killing it so that the patient, although he or she will still be sick, is never in critical condition. This could potentially help offset the chance of Staphylococcus aureus defending itself against this strategy by building up resistance – or so the researchers hope.
Another option is bolstering and activating the immune system using therapeutic antibodies. These antibodies are used to label the bacteria, in turn making the latter more visible for detection by the immune system and the body’s defender cells. Essentially, help the body help itself.
Staphylococcus aureus as permanent guest
Even in cases of mild infections caused by the bacterium, the immune system is not always able to permanently rid itself of the infection. At a certain point, our immune system simply surrenders its weapons – abandoning production of defender cells and thus giving the pathogen a chance to permanently set up shop inside its host undetected. The problem here is that the pathogen will continue to come out of its hiding place periodically to trigger a serious infection only to withdraw into hiding again afterwards.
It is impossible to fight these chronic infections with antibiotics as the drugs are not able to penetrate the intracellular hiding places. This, then, is another one of our scientists’ research emphases – looking for ways to activate the immune system so as to enable it to get caught up with the bacteria, even if defeat itself remains elusive.
Dangerous resistances
Staphylococcus aureus has evolved a number of strategies to help shield itself from antibiotics. At this point, traditional antibiotics are only effective against a small number of bacterial strains as many strains have already evolved resistance to the most commonly administered drugs. Only certain antibiotics still work against a small number of Staphylococcus aureus strains, and many have become almost completely ineffective. The resistant strains are called MRSA’s, an acronym which stands for “methicillin-resistant Staphylococcus aureus.“ Methicillin is a test antibiotic used to determine the sensitivity of pathogens to different antibiotics. Germs that are resistant to this test drug are typically also resistant to most traditional antibiotics. In such cases, it is only vancomycin that can still be used against MRSA’s; although mutant strains of Staphylococcus aureus have since been discovered that are even resistant to vancomycin.
Home: the hospital
MRSA’s are also known as hospital germs as they frequently lead to problems in hospital settings – where people with already weakened immune systems are easy targets for staphylococcus. MRSA germs have been spreading rapidly over the last few years using different routes of transmission. New studies have found that they even are prominent visitors to nursing homes. HZI scientists are also conducting population studies to determine the extent to which MRSA germs have already spread among healthy individuals in “normal” everyday settings.
(jsg)