Vaccination
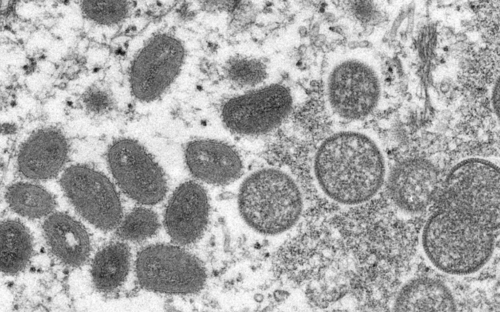
The development of immunisations is considered to be one of the most significant medical achievements of the 20th century. Smallpox for example has been eradicated since the late 70s as a consequence of a successful worldwide vaccination programme.
As early as in the late 18th century, the English physician Edward Jenner proved that an infection involving the cowpox virus – which are comparatively harmless for humans – could protect them from genuine smallpox. He is thus considered the founder of active immunisation. By administering weakened or dead pathogens, or fragments thereof, the immune system of the vaccinated individual is stimulated to form antibodies. Conversely, passive immunisation involves the administration of previously prepared antibodies. These “post-exposition-prophylaxes” are given to patients, for example, after they have been bitten by animals suspected of being infected with rabies.
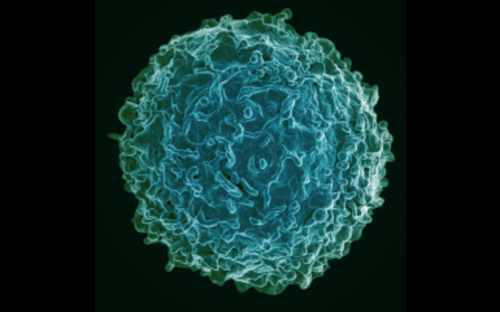
Most vaccines are injected into a muscle. Usually, the antigens that are supposed to elicit the immune response are administered directly. Vector and mRNA vaccines, on the other hand, contain the genetic blueprint for the antigen, which is produced by the body cells that have absorbed the vaccines. The basis for the activation of the immune system are specialised immune cells - the antigen-presenting cells. These sit in the tissue and, once they have recognised foreign structures, migrate to the lymph nodes - the control centres of the immune system. After vaccination, the antigen-presenting cells trigger an alarm in the immune system. They release various signalling substances and place fragments of the antigen on their surface. In this way, they show the B and T cells who the invader is that needs to be fought off.
These cell types form the two arms of the acquired immune system, the cellular arm with T cells and the humoral arm with B cells. A subpopulation of the T-cells is specialised in seeking out and destroying virus-infected body cells so that the virus cannot reproduce further. B cells produce antibodies against antigen that was given by vaccination. These spread throughout the body with the blood and render invading pathogens harmless. By activating both T cells and B cells, vaccinations promise good and lasting protection against disease.
Some time after vaccination, the reaction subsides. However, vaccinated people retain antibodies in their blood for a long time, as well as some T and B cells that remember and can react quickly when they are really infected with the pathogen. B cells then turn back into highly productive factories for antibodies when an alarm signal is given. T cells are activated to seek out infected cells.
The direct link between vaccination and disease control can be observed very well in Germany.“Oral vaccination is sweet – infantile paralysis is terrible” – this slogan was used in the Federal Republic of Germany as an advertisement for poliomyelitis oral vaccination. As proof of its great success, the number of those infected in Germany decreased, according to data from the Paul Ehrlich Institute, from more than 5,600 in 1961 to less than 300 in the first year after the introduction of the vaccination. Nowadays, Germany, as well as the rest of Europe, is considered to be polio-free and the vaccine is one component of a combination immunisation.
In 2014, only Nigeria, Afghanistan and Pakistan remain polio-endemic. Where infantile polio has not yet been conquered, it continues to be administered in liquid form. Consequently, no new needle is required for each individual to be vaccinated, nor are specifically-trained medical personnel necessary. This is ideal in regions of the world in which the nearest hospital can be a few hundred kilometres away.

This is also the case for a kind of vaccination which is currently being developed by researchers at the HZI: The vaccine is in this case administered as a nasal spray. This means the immune reaction can take place directly in the nasal mucous membrane, where many pathogens would also enter into the body later on. This form of vaccination needs no painful “prick” of the needle, which is feared by many and can even cause them to shirk vaccinations altogether. This vaccine fatigue is problematic, as only a high number of vaccinated individuals among the population leads to a so-called “herd immunity”. Pathogens can hardly be disseminated further, thus there is also protection for those who weren’t able to be vaccinated and for those whose vaccinations failed, e.g. individuals with pre-existing diseases or immune-defects, or children prior to vaccination.
For measles, Germany has introduced a mandatory vaccination for some groups of people in 2020. It applies to children from the age of one when they enter kindergarten or school and to employees of social or medical institutions (e.g. educators, teachers, medical staff).
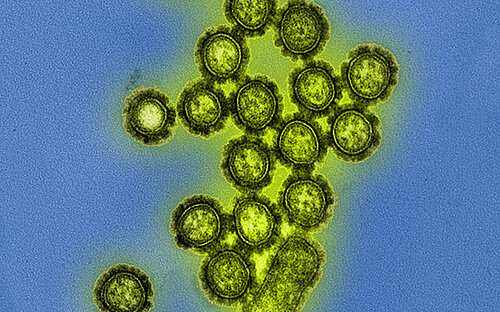
An annually recurring vaccination is that against influenza. The influenza virus that triggers this disease is able to change its surface structures very quickly. This makes it difficult for our immune system to recognise and eliminate new variants of these viruses. New virus variants, against which we have no immunity, emerge about every two to three years. The vaccine must therefore be adapted to the new variants every year. After vaccination, it takes about 14 days for the vaccine protection to build up. The STIKO (Standing Committee on Vaccination at the Robert Koch Institute) recommends the annual flu vaccination for all people over 60 years of age, for people with chronic illnesses that make it more likely that they will contract the flu or that its course may be more severe, as well as for medical and nursing staff.
(bma, Ulrike Schneeweiß)
Involved research groups
-
Antiviral Antibody-Omics
 Prof Dr Yannic Bartsch
Prof Dr Yannic Bartsch -
Experimental Virology
 Prof Dr Thomas Pietschmann
Prof Dr Thomas Pietschmann -
Early Life Immunity
 Dr Natalia Torow
Dr Natalia Torow -
Vaccinology and Applied Microbiology
 Prof Dr Carlos A. Guzmán
Prof Dr Carlos A. Guzmán -
Viral Immunology
 Prof Dr Dr Luka Cicin-Sain
Prof Dr Dr Luka Cicin-Sain