The steadily increasing resistance of many pathogens to antibiotics is one of the major challenges of modern medicine. Many of the common antibiotics have already lost their effect. Accordingly, there is an urgent need for alternatives to antibiotics for the treatment of infections that are caused by multi-resistant bacteria, one of which is anti-virulence therapy. Anti-virulence therapies aim to attenuate those properties of a pathogen that enable its successful infection of the body – the so-called virulence factors – by specific drugs.
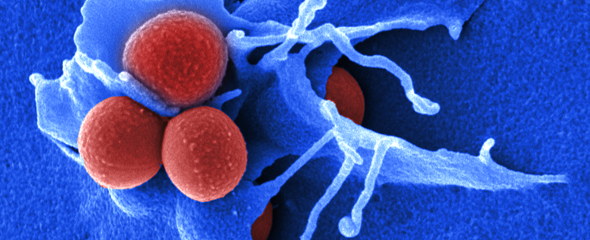
To test the applicability of these anti-virulence strategies, HZI researchers used modern sequencing methods to decipher the interplay of bacteria and the host immune system in experimentally infected mice. Using Staphylococcus aureus as their test pathogen, they discovered that differences in the immune response of mice and the ensuing differences in the course of disease have a strong influence on the specific manifestation of the pathogen’s virulence factors. This, in turn, impacts the effectiveness of anti-virulence strategies. Since the immune response of humans also varies from one individual to the next, these results show that the implementation of anti-virulence therapies in clinical settings will be more successful in the scope of a personalised infection medicine. The researchers published their results in Nature Communications.
The incidence of infections caused by multi-resistant pathogens is on the rise throughout the world; these infections can lead to severe complications, e.g. following surgeries on the joints, chemotherapy or in the management of premature infants. According to current figures, more than 700,000 people each year succumb to infections caused by antibiotic resistant pathogens. For this reason, many researchers investigate new antibiotics as well as alternative antimicrobial medications. One particularly attractive option is the so-called anti-virulence therapy, which aims to use specific drugs to disable certain virulence factors of a pathogen but without directly killing the pathogen. For example, anti-virulence drugs can block adhesion molecules needed by the pathogen to attach to the host tissue or can interfere with bacterial communication signals –the so-called quorum sensing molecules – that allow bacteria to share information during infection. The scientists aim to use this strategy to interfere with bacterial pathogens during an infection, so that they are no longer capable to effectively colonise the body and cause infection.
"The anti-virulence therapy, either alone or with the help of an antibiotic, weakens the pathogen and helps the immune system to defeat the infection," says Prof Eva Medina, who is the head of the Infection Immunology department at the HZI. "Since the pathogens remain alive and capable of proliferation, there is no selection pressure that would drive the development of resistance." However, she says that the concept of anti-virulence therapy is still in its infancy and that more research is needed to translate it into clinical applications. "One very important aspect to be considered during the development of new anti-virulence concepts is the fact that virulence factors are not always expressed in the same way by the pathogens. The specific expression level of these factors is strongly influenced by the environment encountered during the infection," says Medina. “It is therefore important to determine if differences in the host’s immune response, which is highly variable among individuals, influence the pathogens expression of virulence factors.” The HZI scientists recently studied this aspect using the major nosocomial pathogen, Staphylococcus aureus.
"For the study, we conducted infection experiments with various mouse lines," says Robert Thänert, a scientist in the team of Eva Medina. "One of the mouse lines we investigated was highly susceptible to Staphylococcus aureus infection and infected mice developed severe sepsis. In contrast, a second mouse line showed only mild disease symptoms." The subsequent sequencing of the RNA from infected tissue – i.e. the entire set of all active genes – made it possible, for the first time, to determine the genetic activity of both the host and the pathogen during an ongoing infection.
Eva Medina adds: "Combining the RNA profiles of the pathogen with that of a resistant and a susceptible host, we were able to show that differences in the immune response of the host do in fact have an impact on the gene activity of Staphylococcus aureus during the infection. The variability in the severity of Staphylococcus aureus infection that we observed in mice has also been seen in humans and may result from differences in age or in the specific genetic makeup."
However, the fact that the expression of virulence factors by pathogens depends on the host might actually limit the effective application of anti-virulence therapies. "This is very important information for the development of functional anti-virulence concepts," says Eva Medina. "Ideally, anti-virulence therapy should target pathogenic factors of bacteria that are regulated independently of the host." Unless this is the case, anti-virulence strategies need to be specifically adapted to the individual patient. The HZI researchers say that the experiments performed with Staphylococcus aureus can be, on principle, translated to other pathogens for addressing the use of anti-virulence therapy as treatment modality in clinical settings.
Original publication:
Robert Thänert, Oliver Goldmann, Andreas Beineke and Eva Medina: Host-inherent variability influences the transcriptional response of Staphylococcus aureus during in vivo infection. Nature Communications, 2017; DOI: 10.1038/NCOMMS14268