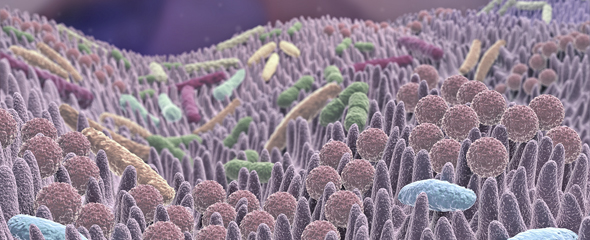
Intestinal bacteria are an important component of digestion as they convert food items into substances that can be absorbed by the body. But sometimes, the activity of these bacteria may be harmful to the human body. Certain bacterial degradation products promote the development of atherosclerosis, a risk factor of cardiovascular diseases such as stroke or heart attacks. To name one example: Meat and eggs contain high concentrations of a substance called choline. In addition, red meat contains carnitine as well. Both molecules can be metabolised by intestinal bacteria to produce the same substance, trimethylamine (TMA), which is subsequently oxidised to trimethylamine-N-oxide (TMAO) in the liver. This compound promotes the uptake of cholesterol into certain immune cells, which leads to the formation of plaque that contributes to the development of atherosclerosis.
"There existed already much information about TMA and its influence on human health, but very little was known about the abundance and the specific composition of the corresponding microbial communities in the gut," says Dr Marius Vital, who is a scientist with the HZI's "Microbial Interactions and Processes" research group. "This can be explained, on the one hand, by the low abundance of TMA producers in the intestines - but mainly by the lack of specific methods for their quantification in the past."
The HZI researchers therefore developed a sensitive method that allows measuring the TMA-producing potential of microbial intestinal communities in ordert o gain new insights into the detailed composition of this important functional group.
To this end, the researchers analysed human stool samples from 50 volunteers, who did not meet any health-related exclusion criteria. First, they established a gene database for the most important key enzymes of the TMA synthesis pathway based on 70,000 publicly accessible genomes. Then they developed gene-specific assays for the respective key enzymes allowing the identification of bacteria to produce trimethylamine based on their genetic ability.
"Using the molecular biology-based search for TMA key enzymes - without culture - we were able to quantify bacteria in the intestines that all are potentially capable of producing trimethylamine. We recognised, by sequencing, that some of these were unknown bacteria that are related to certain Clostridia," says Marius Vital.
The newly developed diagnostic workup now allows us to discover specific risk groups and assist the design of therapies for specific changes to the intestinal flora. The application of pro- and pre-biotics, as well as faecal transplantation, is imaginable. "We are still at the very beginning and it will take many studies to better understand the exact mechanisms," says Vital.
In the future, the researchers will collaborate with colleagues from Greifswald and conduct comprehensive analyses in the course of a cohort study, in which scientists from the "Epidemiology" and "Chemical Biology" research groups of the HZI will participate as well.
The scientists hope to gain more detailed insights into the relationships between nutrition, intestinal flora and cardiovascular diseases. These results might contribute to the development of specific therapies preventing the production of TMA and cardiovascular diseases.
Original publication:
Rath, S., Heidrich, B., Pieper, D. H., & Vital, M. (2017). Uncovering the trimethylamine-producing bacteria of the human gut microbiota. Microbiome, 5, 54. http://doi.org/10.1186/s40168-017-0271-9