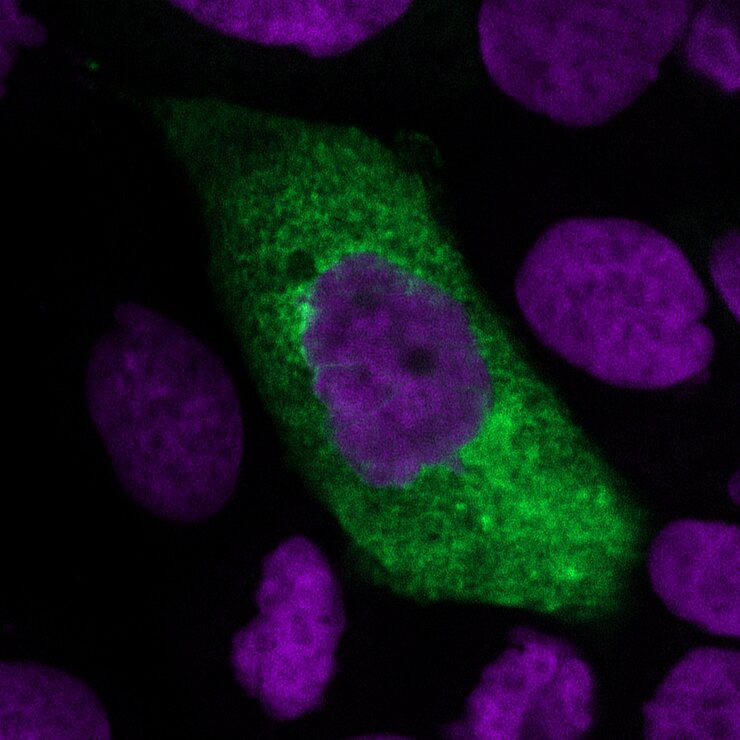
Virus particles are tiny – 20 to 300 nanometres in diameter and thus about 1000 times smaller than a human cell. They consist of little more than their genetic material and a protective protein shell. They even save their own metabolism and use their host’s instead. Once they have invaded a host cell, they reprogram it. The cell reads the viral genome, multiplies it and produces viral proteins. Thus, the host cell produces more and more viral particles until it dies, thereby releasing the viruses.

New viruses, new challenges
Into the host – and out again
However, viruses cannot simply invade a new host such as humans. They need a “key” to enter its cells. “To do this, viruses use proteins on our cell surface. They can only infect us if these proteins match the proteins on the virus surface,” says Prof Luka Cicin-Sain, head of the research group “Immune Aging and Chronic Infections” at the Helmholtz Centre for Infection Research (HZI). But not all host cells have the right “lock” on their surface: Viruses can only multiply in a tissue whose cells produce receptors that match the virus. This results in the migration of viruses into individual organs – influenza viruses multiply in the lungs and bronchial tubes, hepatitis viruses live in the liver and the human immune deficiency (HI) virus prefers cells of the immune system. In SARS-CoV-2, a surface protein, which scientists call the spike protein, plays the role of the “key”. According to Cicin-Sain, the virus' key step in changing host to humans was a mutation of the spike protein that now enables SARS-CoV-2 to bind to the ACE2 receptor on human cells.
The place where a virus shelters is also crucial for its further spread. “Getting into the body and multiplying there is one thing – but in order to spread further, viruses must also get out of the host,” says Cicin-Sain. Viruses that multiply in the airways or the digestive tract have it easier than those that occur in internal organs or the bloodstream.
“When a new, unknown virus appears, it is obvious to check whether it belongs to one of the virus families from which new viruses have emerged in the past. These are usually viruses whose genetic material consists of RNA,” says Luka Cicin-Sain. Depending on the structure of their genetic material, viruses have different prerequisites for changing hosts. RNA viruses change faster genetically than viruses with a DNA genome. This is because the protein that multiplies the RNA often incorporates small defects. The mutations in the genetic material result in different virus variants, which differ slightly. Therefore, RNA viruses adapt to a host faster than DNA viruses.
Using mosquitoes to get to the host
Some viruses use assistants to move from person to person. For example, bloodsucking animals such as mosquitoes or ticks can absorb viruses whilst feeding. These multiply in the animals and are transferred back to a human host with another bite. This is why mosquitoes were involved in an epidemic in which a virus did not have to newly cross the species barrier, the Zika epidemic. This virus has been known since the 1950s. However, mass illness did not occur until the Zika virus was introduced to Central and South America in 2015 and conquered a new continent thanks to mosquitoes. “A prerequisite for the transmission of the Zika virus is that it can multiply in both humans and mosquitoes – two completely different species. This is an enormously complex system where the transition between two species must take place again and again,” says Luka Cicin-Sain. A completely new virus that spreads to another species with the help of mosquitoes could then spread to humans instead. The West Nile virus is an observed example of this. The virus, which is transmitted by mosquitoes, normally circulates between mosquitoes and birds, but it can also infect humans and other mammals.
Concentrating on certain host species is a typical characteristic of viruses – but this varies in severity depending on the virus family. “We know of both generalists and specialists among the viruses. The specialists are confined to a single host, whereas generalist viruses can change hosts more easily,” says Luka Cicin-Sain. With his team, he is conducting research on the cytomegalovirus (CMV), a virus that is highly specialised in humans. CMV, which belongs to the herpes virus family, has completely adapted its lifestyle to humans. Such highly specialised viruses carry the blueprint for many proteins that interact with the human immune system in their genome. With the help of these proteins, they can switch off the immune defence and prevent infected cells from being destroyed. Thus, CMV can survive unnoticed by the immune system for many decades in human cells. In up to 90 percent of the population, this virus lies dormant in the body without causing symptoms. The immune system keeps the pathogen in check to such an extent that no active infection breaks out. “However, such an interplay does not arise out of nowhere, but is the result of a very long adaptation to a host. In contrast, generalist and new viruses cannot permanently hide from the immune system,” says Luka Cicin-Sain. This would make it easier to develop a vaccine against such viruses.
No single solution for vaccinations
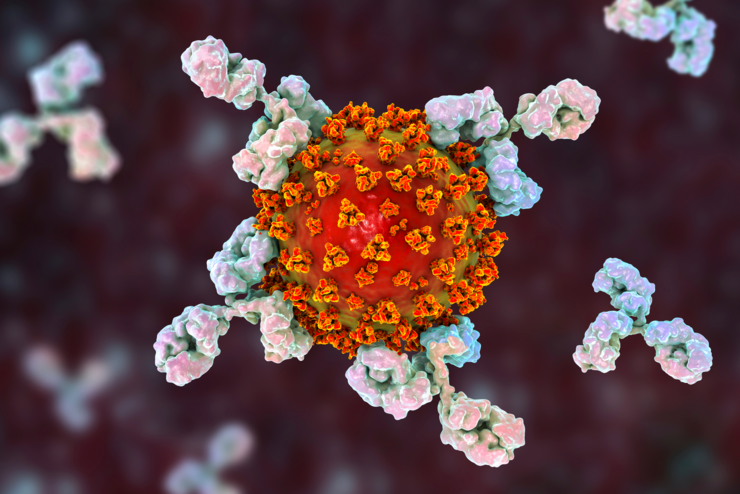
What can we do in future to stop new viruses that have already made the leap to humans? An important element is the rapid development of a vaccine. Vaccination trains the immune system to deal with a pathogen without a previous disease. An infection is imitated, so to speak. In case of a later encounter with the pathogen, the immune system can quickly recall the experience and prevent infection. While broad-spectrum antibiotics are available to fight bacterial infections and research for an equivalent against viruses – i.e. broadly effective antiviral drugs – is also being conducted, there is no such thing as a universal vaccination. “Our immune system is a master in triggering highly precise immune reactions specifically directed against a pathogen. This is why known vaccines cannot be converted so easily,” says Prof Carlos A. Guzmán, head of the department “Vaccinology and Applied Microbiology” at HZI.
“Fortunately, with SARS-CoV-2 we did not have to start from scratch. There has already been intensive research into vaccination against SARS and MERS coronaviruses,” says Guzmán. So scientists already knew that the spike protein was a good target for vaccine development. If a vaccination uses this protein as an antigen, it stimulates the immune system to produce antibodies against it. On contact with the virus, the antibodies make the spike protein, the virus key, inaccessible and thus block its way into the cells.
However, not every virus emerging in the future will be as closely related to already known pathogens as in the current case of SARS-CoV-2. Moreover, as it is impossible to predict which virus will be transmitted to humans next, vaccine research focuses on technical development: “Reverse vaccinology has literally turned the research process upside down,” says Carlos Guzmán. Traditionally, pathogens were characterised in lengthy fundamental research. For example, scientists investigate which mechanisms a pathogen uses to trigger a disease or which of its structures are particularly well recognised by the immune system. Vaccine development then builds on this knowledge. In contrast, reverse vaccinology is based on the genetic code of a pathogen, which can be determined very quickly using modern sequencing technology. In the case of SARS-CoV-2, the genetic code was already decoded and available in a database in mid-January 2020 – at a time when only a few dozen infections were known. “Having this dataset meant that vaccine research could start immediately without having to grow the virus in the laboratory or examine it in any other way,” says Guzmán. In such cases, computer-based approaches help to select the best antigen for a vaccine.
Vaccines must then go through a long development and optimisation process. “Normally it takes about ten years to develop and approve a vaccine,” says Carlos Guzmán.
“With the SARS-CoV-2 vaccination, science is exploring the limits of how much the process can be accelerated. However, safety must under no circumstances fall by the wayside.”
Eventually the vaccination against SARS-CoV-2 would be administered to a large proportion of the population. Even rare serious side effects would then affect a large number of people.
Never-ending cycle
Even in the Stone Age, viruses were our companions – and they will remain so in the future. “The reservoir of viruses in the animal kingdom is almost infinite. Sooner or later, it is inevitable that a new virus will spread to humans,” says Luka Cicin-Sain. The challenge will be to get the next wave of disease caused by a new virus under control before it develops into a major epidemic.
Author: Charlotte Wermser
Published: März 2021