Researchers at Cleveland Clinic’s Lerner Research Institute and the HZI have reported that their universal flu vaccine candidate elicited a strong immune response and provided protection against severe infection and rapid clearance after viral exposure in ferrets. This new work builds on previous seminal studies from the group led by Ted M. Ross, Ph.D., Director of Global Vaccine Development at Cleveland Clinic to design the antigens, and a mucosal adjuvant developed at the HZI by the team of Prof. Guzman, head of the department “Vaccinology and Applied Microbiology”.
According to virologist Naoko Uno, Ph.D., who led the study at the Cleveland Clinic, the researchers hope to launch human clinical trials within 1-3 years. “We want to make sure our vaccine can span multiple seasons, not just one, and protect against all the strains that affect humans,” she said.
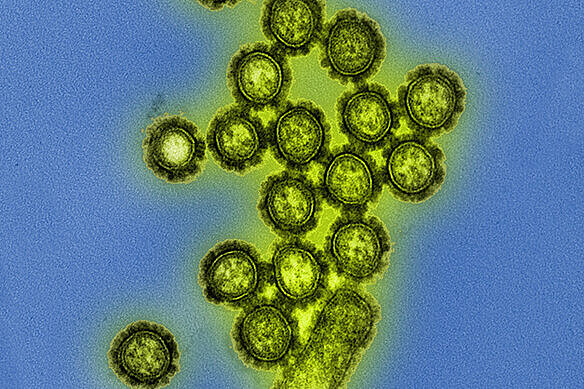
Scientists have identified four types of influenza virus, but two of them—Influenza A and Influenza B—pose the greatest risks to humans. Seasonal flu vaccines include proteins from three or four circulating subtypes of those viruses, which include H1N1, H3N2 and IBV. However, because the virus mutates so quickly, predicting which strains will pose the biggest risk and, thus, choosing which ingredients to include is a guessing game.
Researchers in Ross’ lab designed the new vaccine candidate antigens using a methodology called COBRA (Computationally Optimized Broadly Reactive Antigens). They began by downloading thousands of genetic sequences of pathogenic influenza strains, spanning multiple seasons, from an online database. Then, they digitally analyzed those sequences to identify which amino acids—the building blocks of proteins—are conserved across viruses and seasons.
The researchers identified groups of proteins for different subtypes. To develop a wider-reaching vaccine, the group identified eight proteins from those previous studies associated with a sustained immune response. Uno said, “We have been able to whittle down this list to say these are the best at spanning multiple seasons and eliciting a broadly reactive antibody response. It is like creating a greatest hits album. We want to put only the best ones back in the vaccine.”
Those greatest hits included proteins from H1 and H3 types of influenza viruses, but they also included proteins from H2, H5 and H7 viruses, which are strains against which most people do not have antibodies. Some of these have pandemic potential. Past outbreaks of bird flu (H5N1) have led to a high rate of human mortality, and in March 2024 the virus was found in dairy cattle in Texas, USA. Since then, four people who work with cattle have been diagnosed. In addition, it has spread to dozens of herds in multiple US states, and in other species including sea lions, birds, cats and alpacas. “We’ve shown that our H5 vaccine does cover many different clades,” Uno said.
“As we have seen by SARS-CoV-2, a vaccine which is not able to stimulate a local immune response cannot efficiently protect against infection or transmission”, said Guzman. Thus, before starting the new work, different formulations containing the mucosal adjuvant c-di-AMP developed at the HZI were evaluated after intranasal vaccination in mice. “We were able to identify vaccine formulations stimulating the production of blood and secretory antibodies as well as cellular immunity against the virus, so that the vaccinated mice exposed to the pathogen were protected against infection,” said Dr. Thomas Ebensen from Guzman’s department at HZI. “This allowed us to select the optimal vaccine composition for the ferret studies performed by Uno presented in the publication. We expect that this innovative vaccine able to stimulate mucosal responses will be able to protect both against disease and infection, reducing also the risk of horizontal transfer from infected individuals to susceptible hosts, a critical feature for a pandemic agent,” said Guzman.
![Dr Charlotte Schwenner [Translate to English:] Charlotte Schwenner](/fileadmin/_processed_/6/9/csm_Charlotte_Schwenner_7952cfe0a7.webp)


![[Translate to English:] Press image](/fileadmin/_processed_/1/d/csm_2023_Webnews_Guzman__c_Wiley-VCH_Angewandte_Chemie_766e4cb343.gif)
