The human intestine is home to around 100 trillion bacteria, which is about ten times the number of cells in our entire body. This internal menagerie, known as the microbiota, weighs at least one kilogram and contains over 500 different species of bacteria. What is more, every individual’s microbiota is different – we all have our own unique zoos.
The microbiota helps its host in a number of ways, for example when digesting certain types of food, such as fibres, that the host cannot digest itself. Furthermore, the bacteria in the microbiota produce B vitamins. Although they generate this for their own use, the host is able to absorb the vitamins as well.
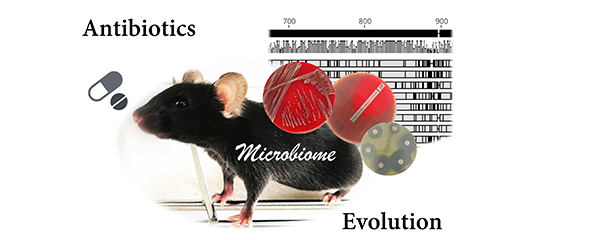
The microbiota also interacts with the immune system and triggers immune reactions in the intestine, as well as in the rest of the body, all the way up to the brain. Keeping the microbiota intact is therefore important for health. However, it is very sensitive to external influences, such as certain diet ingredients and medicines. Antibiotics in particular, though they are essential for fighting life-threatening bacterial infections, affect the "good" bacteria and can kill up to a third of the inhabitants of the gut. This damage is normally short-lived and the microbiota tends to recover in two to four weeks. However, this recovery period can last longer for ill or elderly people and children. The latest studies show that multiple administration of antibiotics in children under the age of three can lead to long-term impairment of the microbiota – this is quite the catch 22, as doctors are more prone to rely on antibiotics for things like middle ear infections during this stage of life. There are often no other alternatives in cases like this.
In hospitals in particular, the frequent use of antibiotics goes hand-in-hand with an increased risk of acquiring pathogens. If the microbiota has been damaged, pathogens like Clostridium difficile, Staphylococcus aureus, Klebsiella pneumoniae or enteropathogenic Escherichia coli exploit this to establish themselves in the gut. C. difficile in particular has gone on to become a major problem for hospitals as it forms environmentally-resistant spores that can survive for months outside of the body. Once they have been absorbed by patients being treated with antibiotics, these spores germinate and produce toxins that paralyse the intestinal wall and, in the worst-case scenario, lead to the balloon-like distention of the large intestine, a life-threatening condition.
These side effects, some of which are very severe, show that antibiotics use is not without harm and alternatives would be desirable – for some areas of application at the very least. One possible approach is the microbiota itself: An increasing number of studies in the USA and the Netherlands are showing that stool transplants can have a similar effect to antibiotics for certain gastrointestinal bacterial infections. Populating the intestines with "good" bacteria leads to the suppression of pathogens and the prevention of new infections. However, this model is also not without risk as transferring a multitude of known and unknown bacteria can have long-term consequences for the recipient. As a result, scientists are currently researching the administration of defined types of bacteria and other completely different treatments, such as the administration of pathogen-specific phages that do not attack the microbiota.
A decisive factor for new approaches to therapy is understanding the interaction between the microbiota, immune system and pathogens. However, it is not actually that easy to accurately study the microbiota: Sequencing, for example, provides a huge quantity of data on all bacteria, known as metagenomics. Information on the individual types of bacteria then has to be filtered out. While there may be many methods of doing so, it is often unclear which one is best for the matter at hand.
In order to solve these problems, an international team of scientists – including Alice McHardy and her HZI department "Computational Biology of Infection Research" at the BRICS in a leading role – founded the initiative "Critical Assessment of Metagenome Interpretation (CAMI)". In the first CAMI-organised benchmarking competition, scientists are able to test and evaluate their computational biology methods on a wide range of metagenomic data sets. "CAMI's aim is to test and analyse methods for metagenomic data under standardised conditions using biologically relevant metrics and to develop standards regarding which method should be used for which scientific problem," says Alice McHardy.