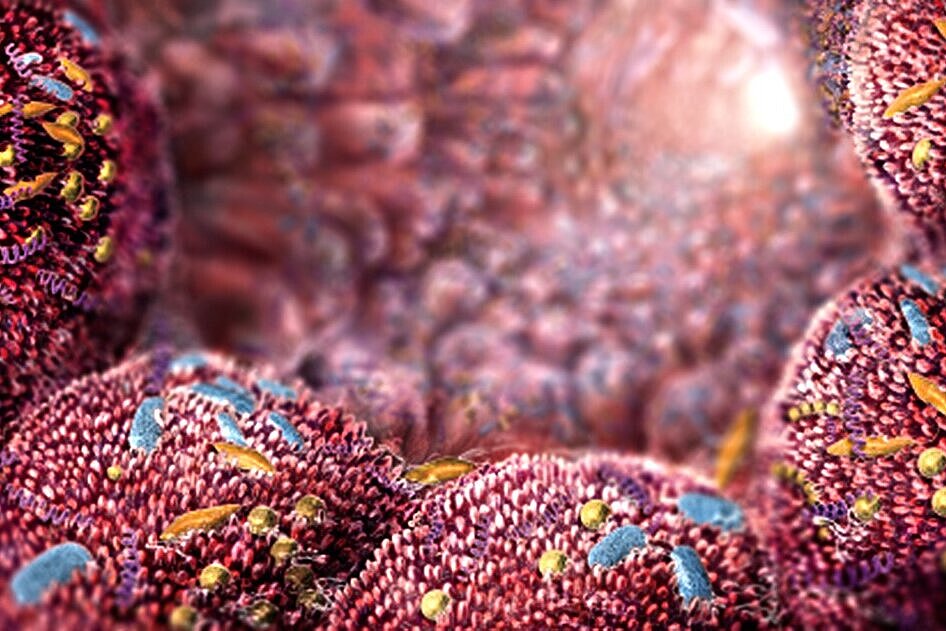
Antibiotics are often the only treatment option for bacterial infections. Generally, however, they have the unfortunate side effect of also killing useful bacteria – for example in the intestine – and thus sometimes disrupting digestion for weeks. For some years now, research into microbiomes, the bacterial communities in and on the human body, has been gaining momentum. It is now known that an intact microbiome strengthens the immune system, influences the course of many diseases and can also protect against infections. With this in mind, the drug researcher Mark Brönstrup and microbiome researcher Till Strowig from the Helmholtz Centre for Infection Research (HZI) discuss whether antibiotics are still relevant today and which findings about the microbiome can be used for treating infections.
What can antibiotic and microbiome researchers learn from each other?
Mark Brönstrup: In the search for new drugs that treat infections, we can learn from the microbiome which mechanisms bacteria use to communicate with each other and to keep each other under control. Bacteria are able to prevent one population from excessive growth and from overwhelming all others in the communities. The strategies to control growth by members of the microbiome could perhaps be used for therapeutic purposes.
Till Strowig: We are interested in how microbial communities affect people, but we also need to understand how members of these communities communicate and compete with each other. Some of the principles used by conventional antibiotics also apply to the microbiome. This is why there are attempts in microbiome research, as an interface to antibiotic research, to identify from DNA sequences of the microbiome how bacteria form their own antibiotic substances. The dominant topic in conjunction with antibiotics is, however, their undesired side effect of damaging the microbiome.