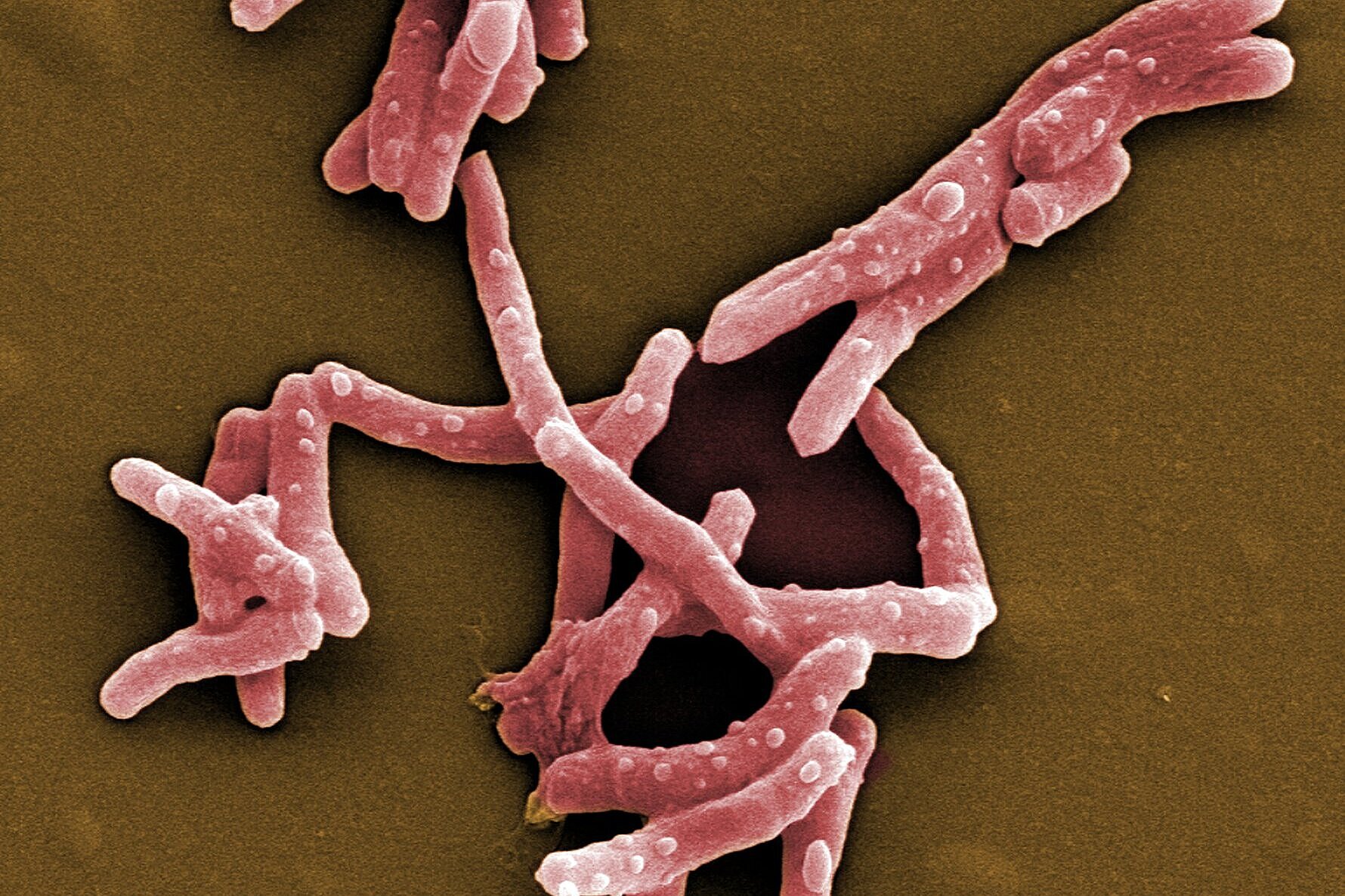
Every year, about 10 million people become infected with tuberculosis and 1.4 million die from it. This makes tuberculosis not only one of the most widespread infectious diseases, but also the deadliest. Similar to malaria or HIV, the prevalence of tuberculosis is strongly dependent on social factors; it is considered a classic disease of the poor. In addition to a lack of medical care, other problems hinder the containment of tuberculosis, such as antibiotic resistance and undesirable drug-drug interactions. The department Microbial Natural Products at the Helmholtz Institute for Pharmaceutical Research Saarland (HIPS), a joint site of Helmholtz Centre for Infection Research (HZI) with Saarland University, is exploring soil bacteria for new active substances to solve these problems. The annual World Tuberculosis Day on March 24 commemorates the discovery of the pathogen Mycobacterium tuberculosis by Robert Koch on this day in 1882.
World Tuberculosis Day 2021: New drugs for old bugs
Tuberculosis is the infectious disease that causes the most deaths every year - in Germany, however, the public hardly notices it. Why is that?
Although tuberculosis (TB) is a worldwide problem, developing countries tend to be hit the hardest. Africa in particular has to contend with a high number of active TB cases and correspondingly high mortality rates. In fact, Europe is the region where the fewest cases are recorded each year. In Europe as a whole, there are circa 300,000 cases per year, while worldwide the number of new infections each year amounts to circa 10 million. At the same time, however, we have the problem in Europe that the relative proportion of multi-resistant strains of the pathogen Mycobacterium tuberculosis is highest here in a global comparison. In Germany, we have not noticed much of this so far; the European hotspots are mainly in Eastern Europe.
How do these infection hotspots emerge? Why is tuberculosis spread so differently?
Tuberculosis is a lung disease and is usually transmitted via droplet infection. Such transmission routes are favored when people have to live under inadequate hygiene conditions or in very crowded conditions. Large outbreaks therefore occur, for example, in refugee shelters or in prisons. Such conditions combined with poverty, where again the health system and medical care are not always adequate, lead to a high spread of TB.
Other pathogens can also spread well under these conditions. How does co-infection with other diseases affect the treatment of TB infection?
Co-infection with HIV is probably the best known example of such a case. This also occurs relatively frequently in practice, since there is a large regional overlap in the spread of these two diseases. Generally speaking, in the case of TB, anything that weakens the immune system can promote the outbreak of the disease and severe progressions. This also includes diseases of civilization such as diabetes. In the case of HIV and TB, there is also the very unfavorable interaction that the two diseases virtually reinforce each other and make treatment even more difficult. The standard treatment of TB already takes a very long time, six months, and can even extend over several years in the case of infections with antibiotic-resistant pathogens. In the case of co-infections, there are also drug-drug interactions. As a result, it is sometimes very difficult to optimally coordinate individual therapies for different infectious diseases.
To solve these problems, the department Microbial Natural Products at HIPS is researching new active substances against the tuberculosis pathogen. How do you go about this?
We prefer to work on molecules to which no resistance exists yet. This means that when we are looking for new molecules, the first step is to test their effect against sensitive bacteria - i.e., those that do not yet exhibit antibiotic resistance. We then investigate whether our drug candidates can also inhibit the growth of resistant strains. If we find complete cross-resistance, i.e. our new active ingredient shows no efficacy against multi-resistant germs, it will be difficult to develop this substance further. However, some of these molecules still offer advantages over other antibiotics available on the market. We have recently investigated one such molecule in more detail: Sorangicin.
What opportunities does Sorangicin offer over other antibiotics?
Like most of our active ingredients, we have isolated Sorangicin from soil-dwelling myxobacteria. Its mode of action is almost identical to that of another antibiotic to which resistance is frequently observed in M. tuberculosis. Both the natural product Sorangicin and the first-line TB drug Rifampicin inhibit RNA polymerase, leading to the death of the pathogen. Since we are not only studying the direct effect on pathogens but also looking at other pharmacological properties, we were further interested in the natural product class. Rifampicin binds to a specific enzyme in the human body, thereby accelerating the breakdown of other drugs. This effect is much weaker in Sorangicin. The natural substance could therefore be a good drug candidate for the development of a TB drug, particularly for use in patients with co-infections, since Sorangicin is less likely to weaken the effect of other drugs. In the course of our research, we also found that Sorangicin may be effective against antibiotic-resistant strains after all. In non-resistant M. tuberculosis strains, Sorangicin and Rifampicin show the same mode of action. When Rifampicin resistance is present, it is due to a mutated binding site in the RNA polymerase. Excitingly, Sorangicin can adapt to this and it also inhibits the mutated enzyme, but via an altered mechanism.
Your department is also currently searching for new active substances against tuberculosis as part of a cooperation project with the company Evotec. What exactly is the project about?
The specific aim of the project is to identify at least one new lead structure within three years and to evaluate it according to pharmacological parameters. Such a lead structure is then typically further optimized in order to be able to enter clinical testing in a timely manner. Together, we are looking for compounds that show good efficacy against M. tuberculosis - also against multi-drug resistant pathogens -, show in vivo efficacy against TB and are also well tolerated by humans. In particular, tolerability is very important for TB drugs, as patients have to be treated for many months. Ideally, we would find a new active substance that might even make it possible to shorten the duration of therapy. The very close cooperation with the company Evotec makes it possible to successfully master such an extensive project. In particular, the participating scientists from HZI and HIPS contribute their expertise in finding and producing new natural products from myxobacteria, with Evotec contributing new technologies. Once we have characterized a promising natural product, we work together on the chemical-synthetic optimization of the natural products, and both partners contribute their expertise in medicinal chemistry. Evotec's resources then play a role for us primarily in the investigation of pharmacological parameters. In this phase, we will contribute more mechanistic studies, i.e. determine where exactly in the cell the targets for the antibiotic are located.
Further Information
Interview: Helen Looney
![Dr Charlotte Schwenner [Translate to English:] Charlotte Schwenner](/fileadmin/_processed_/6/9/csm_Charlotte_Schwenner_7952cfe0a7.webp)
