Innate Immunity and Infection

Our Research
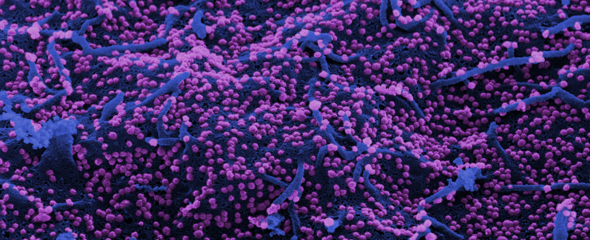
a. Identification of the cell-specific defense of astrocytes during tick-borne encephalitis (TBE) infection. Using cell-specific labeling of newly synthesized proteins in vivo, we investigate changes in gene expression throughout the course of the infection.
b. Cell- and region-specific regulation of type I interferons (IFNs) in the brain.
c. Alterations in brain structure and function following infections with respiratory and neurotropic viruses. Additionally, changes in brain development during infections occurring during pregnancy.
Immune Defense in the Brain: Cell-Specific Responses to Viral Threats
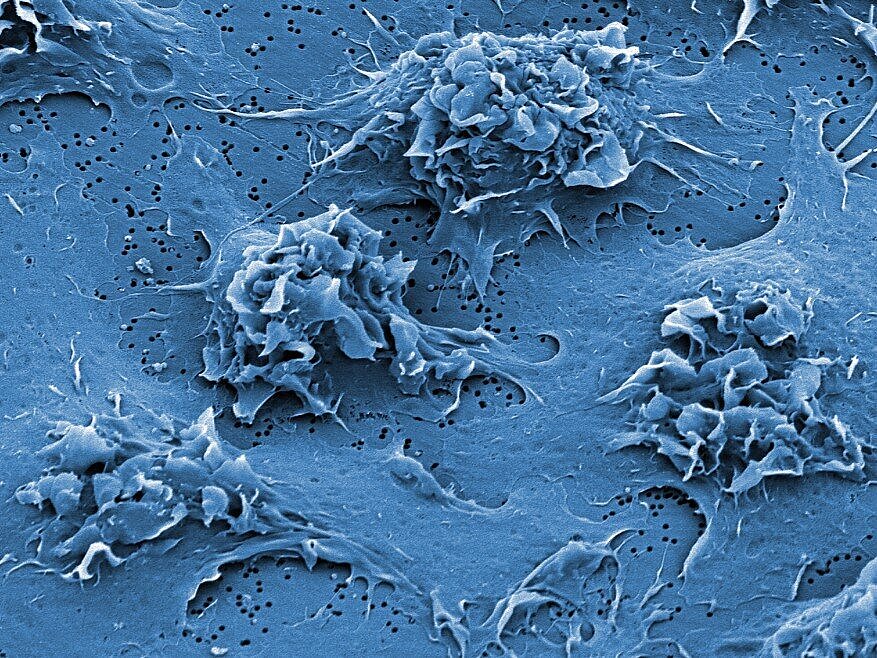
Viral infections in the brain can have devastating consequences, potentially triggering neurodegenerative processes. A well-regulated immune response is therefore essential to protect neural function and maintain homeostasis. Our research focuses on understanding both innate and adaptive immune reactions to viral infections in the brain. Given the complex interplay between different cell types in the central nervous system, we employ cell-specific labeling of newly synthesized proteins to study astrocyte responses during the course of infection. By analyzing these dynamic interactions, our data provide critical insights into how different cell populations contribute to the brain’s defense mechanisms. This knowledge lays the foundation for identifying key intervention points to modulate immune responses and mitigate infection-induced damage.
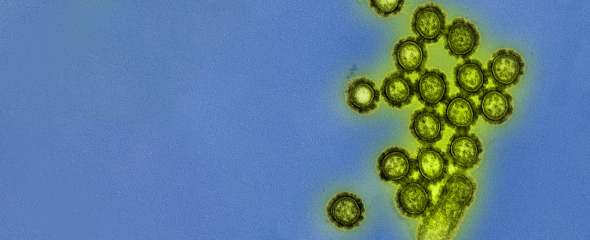
Spezialized Type I Interferon Response in the Brain
Unlike peripheral tissues, the brain exhibits highly specialized regulation of type I IFN responses, both at the level of distinct cell types—such as neurons, astrocytes, and microglia—and across different brain regions. This spatially restricted IFN signaling ensures effective viral control while minimizing neuroinflammation and preserving neural function. Neurons often exhibit a tightly controlled, low-level IFN response, while glial cells can mount robust antiviral defenses. Moreover, brain region-specific differences in IFN activity suggest a finely tuned immune surveillance system adapted to local cellular environments. We aim to understand these unique regulatory mechanisms in different cell types as essential for developing targeted therapies against neurotropic viral infections.
Viral Disruption of Biological Barrieres
Viral infections can profoundly influence antiviral responses not only within tissues but also at critical biological barriers, including the blood-brain barrier, choroid plexus, meninges, and placenta. These effects may result from direct viral action or indirectly through inflammation-induced disruption. Compromise of such barriers facilitates viral entry into the central nervous system and, in pregnant individuals, transmission to the developing embryo. Infections during key stages of development can lead to lasting alterations in brain structure and function, with potential long-term neurological consequences. Elucidating the mechanisms by which viruses breach and impair these protective barriers is crucial for designing strategies to prevent vertical transmission and safeguard the central nervous system.
Our Research
a. Identification of the cell-specific defense of astrocytes during tick-borne encephalitis (TBE) infection. Using cell-specific labeling of newly synthesized proteins in vivo, we investigate changes in gene expression throughout the course of the infection.
b. Cell- and region-specific regulation of type I interferons (IFNs) in the brain.
c. Alterations in brain structure and function following infections with respiratory and neurotropic viruses. Additionally, changes in brain development during infections occurring during pregnancy.
Immune Defense in the Brain: Cell-Specific Responses to Viral Threats
Viral infections in the brain can have devastating consequences, potentially triggering neurodegenerative processes. A well-regulated immune response is therefore essential to protect neural function and maintain homeostasis. Our research focuses on understanding both innate and adaptive immune reactions to viral infections in the brain. Given the complex interplay between different cell types in the central nervous system, we employ cell-specific labeling of newly synthesized proteins to study astrocyte responses during the course of infection. By analyzing these dynamic interactions, our data provide critical insights into how different cell populations contribute to the brain’s defense mechanisms. This knowledge lays the foundation for identifying key intervention points to modulate immune responses and mitigate infection-induced damage.
Spezialized Type I Interferon Response in the Brain
Unlike peripheral tissues, the brain exhibits highly specialized regulation of type I IFN responses, both at the level of distinct cell types—such as neurons, astrocytes, and microglia—and across different brain regions. This spatially restricted IFN signaling ensures effective viral control while minimizing neuroinflammation and preserving neural function. Neurons often exhibit a tightly controlled, low-level IFN response, while glial cells can mount robust antiviral defenses. Moreover, brain region-specific differences in IFN activity suggest a finely tuned immune surveillance system adapted to local cellular environments. We aim to understand these unique regulatory mechanisms in different cell types as essential for developing targeted therapies against neurotropic viral infections.
Viral Disruption of Biological Barrieres
Viral infections can profoundly influence antiviral responses not only within tissues but also at critical biological barriers, including the blood-brain barrier, choroid plexus, meninges, and placenta. These effects may result from direct viral action or indirectly through inflammation-induced disruption. Compromise of such barriers facilitates viral entry into the central nervous system and, in pregnant individuals, transmission to the developing embryo. Infections during key stages of development can lead to lasting alterations in brain structure and function, with potential long-term neurological consequences. Elucidating the mechanisms by which viruses breach and impair these protective barriers is crucial for designing strategies to prevent vertical transmission and safeguard the central nervous system.
Prof Dr Andrea Kröger
A pathogen’s initial contact with the host is crucial for the outcome of an infection. The host’s initial reactions will decide whether the host is able to assert itself or whether it will lead to a chronic infection and more serious illness.

Andrea Kröger received her initial training in Biology during her studies of Biology at the Technical University of Braunschweig. 1995, she joined group of Dr. Hansjörg Hauser at the Department of Gene Regulation and Differentiation of the Helmholtz Centre for Infection Research. During her doctoral studies, she worked on the characterization of suppressive effects of the transcription factor IRF-1 in mouse tumor models and the development of screening cell lines for the identification of small molecules for IRF-1 induction.
During her postdoctoral studies in Dr. Hansjörg Hauser´s group, her research focuses on stimulation of the immune response. Since 2010, as principal investigator of the “Interferons in Immune Defense and Immunity“ project, Andrea Kröger is searching for the mechanisms used by the interferon system to fight infections and influence protective immune responses.
Since 2012Andrea Kröger leads the research group “Innate Immunity and Infection” at the HZI. In December 2014 she completed her habilitation thesis for cell biology at the Technical University Braunschweig. Since June 2015 Andrea Kröger has a professorship for molecular Microbiology at the Otto-von-Guericke-University in Magdeburg.
Team







Selected Publications
Weichert L, Düsedau HP, Fritzsch D, Schreier S, Scharf A, Grashoff M, et al. Astrocytes evoke a robust IRF7-independent type I interferon response upon neurotropic viral infection. J Neuroinflammation. 2023;20(1):213. DOI: 10.1186/s12974-023-02892-w
Jakob J, Kröger A, Klawonn F, Bruder D, Jänsch L. Translatome analyses by bio-orthogonal non-canonical amino acid labeling reveal that MR1-activated MAIT cells induce an M1 phenotype and antiviral programming in antigen-presenting monocytes. Front Immunol. 2023;14:1091837. DOI: 10.3389/fimmu.2023.1091837
Lindqvist R, Rosendal E, Weber E, Asghar N, Schreier S, Lenman A, et al. The envelope protein of tick-borne encephalitis virus influences neuron entry, pathogenicity, and vaccine protection. J Neuroinflammation. 2020;17(1):284. DOI: 10.1186/s12974-020-01943-w
Cornelius ADA, Hosseini S, Schreier S, Fritzsch D, Weichert L, Michaelsen-Preusse K, et al. Langat virus infection affects hippocampal neuron morphology and function in mice without disease signs. J Neuroinflammation. 2020;17(1):278. DOI: 10.1186/s12974-020-01951-w
Kurhade C, Schreier S, Lee YP, Zegenhagen L, Hjertqvist M, Dobler G, et al. Correlation of Severity of Human Tick-Borne Encephalitis Virus Disease and Pathogenicity in Mice. Emerg Infect Dis. 2018;24(9):1709-12. DOI: 10.3201/eid2409.171825