Laboratory of Transmission Immunology

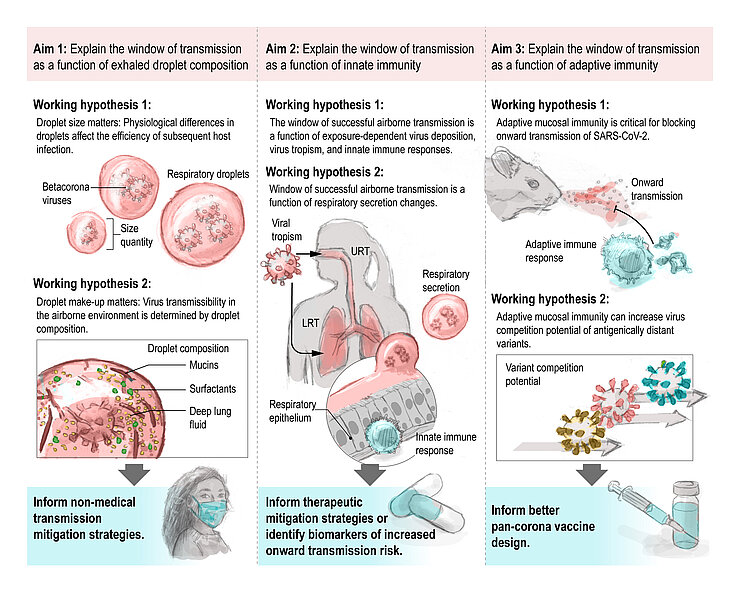
Two of the largest pandemics in the last century, with massive global health and economic impacts, were caused by zoonotic respiratory RNA viruses able to transmit through the air: the 1918 influenza A virus and the betacoronavirus SARS-CoV-2. We know that SARS-CoV-2 is highly efficient at airborne transmission. In comparison, the initial SARS-CoV-1 outbreak was stopped from reaching the same pandemic state because this virus, like Middle Eastern Respiratory Syndrome (MERS)-CoV, presented with less airborne transmission potential. While transmission through respiratory droplets has been posited for all betacoronaviruses, what mechanistically differentiates the transmission potential of these betacoronaviruses is not well understood. Even less is known of more distantly related seasonal human coronaviruses (e.g., HCoV-OC43), which account for up to 35% of adult respiratory infections during peak periods. For respiratory viruses, we do not fully grasp how infection and mucosal immune responses against the infection affect the size, quantity, and physicochemical make-up of droplets in which the virus is exhaled. Therefore, transmission in humans is multifactorial and needs a multidisciplinary rather than a rudimentary experimental approach. To this end, the lab bridges immunology with aerobiology and environmental virology.
The work of the group builds around these three central questions:
- How does immunopathogenesis modulate the window of successful transmission?
- How does pre-existing immunity influence onward transmission?
- How does infection modulate the exhaled or secreted droplets and fluids that carry infectious viruses?
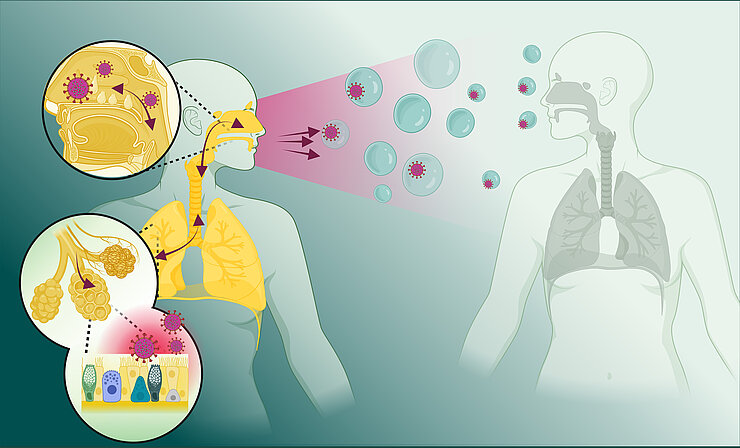
To address these questions, we elucidate the conserved mechanisms of transmission and those that distinguish a highly transmissible virus from a member of the same family (e.g., betacoronaviruses), which caused a self-limited outbreak, using in vitro and ex vivo airway and mucosal models and in vivo transmission studies. We decipher how the site of initial virus replication and subsequent differences in immunopathogenesis and mucus composition impact virus release into the air or bodily secretions.
We study waning cellular and humoral immune responses to viral infections and correlate these immune parameters to the quantity and quality of transmission blockage upon renewed challenge with the same and with related viruses.
Lastly, we investigate whether the quantity and quality of (respiratory) droplets and secretions affect transmissibility. For respiratory viruses, we define the distribution of infectious viruses across different droplet sizes and analyze the exhaled droplet make-up and physicochemical properties, which inform virus stability studies.
This approach will allow us to understand the mechanistic underpinnings of viral transmission and will identify immune signatures linked to an increased risk of onward transmission.
Two of the largest pandemics in the last century, with massive global health and economic impacts, were caused by zoonotic respiratory RNA viruses able to transmit through the air: the 1918 influenza A virus and the betacoronavirus SARS-CoV-2. We know that SARS-CoV-2 is highly efficient at airborne transmission. In comparison, the initial SARS-CoV-1 outbreak was stopped from reaching the same pandemic state because this virus, like Middle Eastern Respiratory Syndrome (MERS)-CoV, presented with less airborne transmission potential. While transmission through respiratory droplets has been posited for all betacoronaviruses, what mechanistically differentiates the transmission potential of these betacoronaviruses is not well understood. Even less is known of more distantly related seasonal human coronaviruses (e.g., HCoV-OC43), which account for up to 35% of adult respiratory infections during peak periods. For respiratory viruses, we do not fully grasp how infection and mucosal immune responses against the infection affect the size, quantity, and physicochemical make-up of droplets in which the virus is exhaled. Therefore, transmission in humans is multifactorial and needs a multidisciplinary rather than a rudimentary experimental approach. To this end, the lab bridges immunology with aerobiology and environmental virology.
The work of the group builds around these three central questions:
- How does immunopathogenesis modulate the window of successful transmission?
- How does pre-existing immunity influence onward transmission?
- How does infection modulate the exhaled or secreted droplets and fluids that carry infectious viruses?
To address these questions, we elucidate the conserved mechanisms of transmission and those that distinguish a highly transmissible virus from a member of the same family (e.g., betacoronaviruses), which caused a self-limited outbreak, using in vitro and ex vivo airway and mucosal models and in vivo transmission studies. We decipher how the site of initial virus replication and subsequent differences in immunopathogenesis and mucus composition impact virus release into the air or bodily secretions.
We study waning cellular and humoral immune responses to viral infections and correlate these immune parameters to the quantity and quality of transmission blockage upon renewed challenge with the same and with related viruses.
Lastly, we investigate whether the quantity and quality of (respiratory) droplets and secretions affect transmissibility. For respiratory viruses, we define the distribution of infectious viruses across different droplet sizes and analyze the exhaled droplet make-up and physicochemical properties, which inform virus stability studies.
This approach will allow us to understand the mechanistic underpinnings of viral transmission and will identify immune signatures linked to an increased risk of onward transmission.
“The field of virus transmission immunology is vastly understudied; we can even argue that it has not left its nascent stage. We will change this”
Julia Rebecca Port was born on September 14th, 1990, in Gelnhausen, Germany. After completing a bachelor's degree at the Eberhard Karls University of Tübingen (Molecular Medicine; B.Sc.) and a master's degree at the University of Antwerp (Biomedical Sciences; M.Sc.), she began her scientific career with her doctorate at the Leibniz Institute for Virology and at the Bernhard Nocht Institute for Tropical Medicine under the direction of Prof. Dr. César Muñoz-Fontela. During her postdoc at the Rocky Mountain Laboratories (NIAID, NIH (USA) in the group of Dr. Vincent Munster, in the department of Dr. Heinz Feldmann), she led experimental projects that addressed urgent public health needs during the SARS-CoV-2 pandemic: this led to the first description of immunopathology following aerosol infection, the first experimental demonstration of fine aerosol transmission, and evidence for an immunity-derived competitiveness in transmission. She also developed models to study the transmission of the Mpox virus across mucosal surfaces and the immune response and microbiome in bats in the context of viral infections. Her research has led to numerous authorships in peer-reviewed journals and has been honored multiple times with the NIH Director's Award and NIH Merit Award. As of May 1st, 2024, Dr. Port accepted the leadership of the new group "Laboratory of Transmission Immunology" at the HZI after successfully acquiring the Helmholtz Young Investigator Grant.
Team




Selected Publications
1. Port, J. R.*, J. C. Riopelle, S. G. Smith, L. Myers, M. C. Lewis, S. Gallogly, A. Okumura, J. E. Schulz, R. Rosenke, J. Prado-Smith, A. Carmody, S. Bane, B. J. Smith, G. Saturday, H. Feldmann, K. Rosenke and V. J. Munster (2023). "Infection with mpox virus via the genital mucosae increases shedding and transmission in the multimammate rat (Mastomys natalensis)" Nature Microbiology. DOI: 10.1038/s41564-024-01666-1
2. Port, J.R., Yinda, C.K., Riopelle, J.C. et al. Infection- or AZD1222 vaccine-mediated immunity reduces SARS-CoV-2 transmission but increases Omicron competitiveness in hamsters. Nat Commun 14, 6592 (2023). DOI: 10.1038/s41467-023-42346-8
3. Port, J.R., Yinda, C.K., Avanzato, V.A. et al. Increased small particle aerosol transmission of B.1.1.7 compared with SARS-CoV-2 lineage A in vivo. Nat Microbiol 7, 213–223 (2022). DOI: 10.1038/s41564-021-01047-y
4. Port, J.R., Yinda, C.K., Owusu, I.O. et al. SARS-CoV-2 disease severity and transmission efficiency is increased for airborne compared to fomite exposure in Syrian hamsters. Nat Commun 12, 4985 (2021). DOI: 10.1038/s41467-021-25156-8
5. Port, J. R.*, D. H. Morris, J. C. Riopelle, C. K. Yinda, V. A. Avanzato, M. G. Holbrook, T. Bushmaker, J. E. Schulz, T. A. Saturday, K. Barbian, C. A. Russell, R. Perry-Gottschalk, C. I. Shaia, C. Martens, J. O. Lloyd-Smith, R. J. Fischer and V. J. Munster (2022). Host and viral determinants of airborne transmission of SARS-CoV-2 in the Syrian hamster, eLife 12:RP87094. DOI: 10.7554/eLife.87094.3
6. Riopelle, J.C., Shamsaddini, A., Holbrook, M.G. et al. Sex differences and individual variability in the captive Jamaican fruit bat (Artibeus jamaicensis) intestinal microbiome and metabolome. Sci Rep 14, 3381 (2024).DOI: 10.1038/s41598-024-53645-5